Are Rescue Breaths Necessary During CPR?

Sudden Cardiac Arrest vs. Heart Attack: What’s the Difference?
June 30, 2023
Teach Your Child to Call 112
June 30, 2023Emergency Care
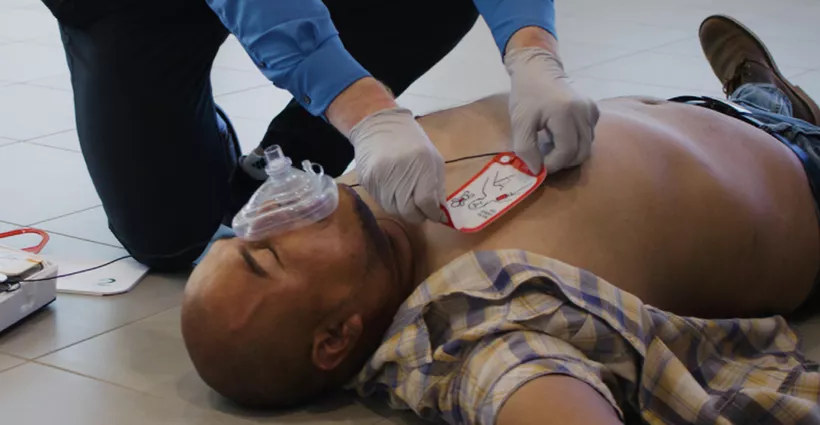
During a cardiac arrest emergency, immediate high-quality cardiopulmonary resuscitation (CPR) improves the chance of survival by providing oxygen-rich blood to the heart and brain. But what does high-quality CPR entail? Are chest compressions enough? Are rescue breaths necessary during CPR?
These are the questions that are frequently asked and addressed in CPR classes across the country.
What is Rescue Breathing?
Sometimes referred to as mouth-to-mouth resuscitation, rescue breathing is a technique used to force air into a person’s lungs. Rescue breathing is typically performed after a person has stopped breathing due to cardiac arrest or an airway obstruction.
Rescue breaths are usually given by exhaling into the mouth or nose of the victim. Whenever possible, barrier protection between the rescuer and the victim should be used.
Why There is Confusion Surrounding Rescue Breaths During CPR
When the 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care were released, one of the underlying goals was to eliminate barriers to action and increase bystander CPR rates by simplifying CPR for untrained bystanders.
This involved supporting compression-only CPR as it simply requires a few minutes to learn and can be easily communicated to the masses, resulting in more people taking action.
However, the primary message that came from the news media was that rescue breaths were eliminated from CPR. Due to this overwhelming messaging, the goal of simplifying CPR for untrained rescuers via compression-only CPR inadvertently created further confusion on the importance of rescue breaths overall.
Years later, public perception hasn’t completely changed as many people still question whether rescue breaths are necessary during CPR.
To help clear up the confusion, here’s how to understand and communicate the importance of rescue breaths to CPR students and the general public.
- For certified lay providers, rescue breaths are critical to performing CPR. CPR training for certification with an authorized instructor should always be taught with rescue breaths to increase the chance of survival.
- For the untrained lay provider, the option to perform compression-only CPR helps to eliminate hesitation or unwillingness to provide care. This also applies to a bystander who has limited personal protective equipment (PPE) or is unwilling to provide rescue breaths out of fear the person may have an infectious disease.
Let’s take a deeper dive into the importance of rescue breaths during CPR.
The Need for Rescue Breaths Varies by Cardiac Arrest Emergency
Cardiac arrest occurs for two primary reasons: sudden cardiac arrest (SCA) and secondary cardiac arrest.
Sudden cardiac arrest (SCA)
The most common is SCA, which happens abruptly when the heart’s electrical system causes the heart to stop pumping, forward blood and oxygen flow ceases, and normal breathing stops. However, uncirculated oxygen remains in the bloodstream.
Research has shown that doing chest compressions without rescue breaths can effectively circulate the remaining oxygen for the first few minutes. Due to this research and other influencing factors — such as the risk of the victim vomiting and properly learning how to give rescue breaths — eliminating rescue breaths appeared to be a reasonable concept.
But the other common path to cardiac arrest, known as secondary cardiac arrest, requires providing effective rescue breaths.
Secondary cardiac arrest
Secondary cardiac arrest happens when an initial airway or breathing problem prevents oxygen from entering the body. This is the most common way cardiac arrest occurs in children. It can be caused by medical emergencies like drowning, suffocation, or opioid overdose.
With secondary cardiac arrest, the lack of available oxygen will progressively weaken and slow the heart rate down until the heart stops. Therefore, getting oxygen into the body becomes critical as it will stimulate the heart to beat faster and become stronger. It will also trigger the resulting oxygen to reach the brain, which can stimulate breathing effort.
SCA and Secondary Cardiac Arrest Emergencies
When we look at SCA vs. secondary cardiac arrest, eliminating rescue breaths for CPR would make providing care more straightforward for a victim of SCA. But it wouldn’t help a victim of secondary cardiac arrest.
Because the cause of medical emergencies cannot always be definitively determined by a lay provider, we must teach traditional CPR with rescue breaths as the gold standard. However, we should also teach compression-only CPR as an alternative option for providing care.
Why Trained Bystanders Should Perform Conventional CPR
Conventional CPR is an emergency procedure that combines chest compressions with rescue breaths to circulate oxygenated blood to the brain and heart, increasing the possibility of successful resuscitation.
High-quality chest compressions are the foundation of high-quality CPR, forcing blood to move from the chest to the lungs, heart, brain, and other vital organs. But rescue breathing — artificial ventilation of the lungs — is also a critical part of CPR as it provides life-sustaining oxygen and ventilation directly to the person’s lungs.
To break it down further, rescue breaths provide both oxygenation of the blood and removal of carbon dioxide. This is done by using the bystander’s own exhaled breath via a CPR mask or through direct mouth-to-mouth resuscitation (if willing and no PPE is available). But how effective is this exhaled breath?
Room air contains about 21% oxygen. Whereas exhaled air contains between 16% and 17% oxygen. Therefore, a bystander’s exhaled breath provides enough oxygen to support life.
In summary, trained CPR providers who are able should perform standard CPR with rescue breaths to improve the chance of survival.
Compression-only CPR is Better Than No CPR
So, what happens if the rescuer isn’t trained in CPR or has limited PPE available? Untrained bystanders or those unwilling to provide rescue breathing can still help by providing compression-only CPR.
Compression-only CPR, sometimes referred to as hands-only CPR, can be an effective alternative and it’s easy to learn.
If a person collapses in front of you, after dialing 911 to ensure medical help is on the way, follow these CPR steps:
- Place the heels of your hands on the center of the person’s chest.
- Push fast and hard.
- Continue giving compressions until trained CPR or emergency medical services providers take over, the automated external defibrillator (AED) directs you to stop while analyzing, or the person shows signs of life (e.g. responding by breathing, moving, or reacting).

Note that compression-only CPR isn’t appropriate or recommended for children and infants. Rescue breaths are extremely important for children and infants because cardiac arrest typically results from asphyxia (e.g. choking on foreign objects, drowning, etc.) rather than having cardiac issues.
Once a child is in cardiac arrest, their oxygen level is already severely depleted, making rescue breaths essential. However, if you’re unwilling or unable to give rescue breaths, performing compression-only CPR is better than no CPR.
CPR Training Saves Lives
CPR training can make a significant difference in being ready and able to respond during an emergency, and it could save a person’s life. Instructor-led CPR training provides students with the opportunity to practice high-quality chest compressions and give rescue breaths for adult, child, and infant scenarios.
A CPR class may also address a variety of medical emergencies and first aid treatments that are often needed in the workplace, at home, in public places, and out in the community.
HSI is a nationally approved and accredited training organization. We provide certification training that is led by authorized instructors. Learn more about CPR, AED, and First Aid training for yourself and your organization with HSI.
Interested in becoming a CPR Instructor or do you already have credentials with another nationally recognized organization? Learn how you can train with HaRA CPR, AED, and First Aid programs.
Original post: HSI